 Staphylococcus aureus - Vulvar Disease - Global Healthcare
Staphylococcus aureus - Vulvar Disease - Global HealthcareWarning: The NCBI website requires JavaScript to operate. Vulvar Abscess Caused by Methicillin-resistant Staphylococcus Aureus (MRSA) in a Postmenopausal WomanTae-Hee Kim1Department of Obstetrics and Gynecology, Soonchunhyang University College of Medicine, Bucheon, Korea. Bel Seap2Department of Maternity, Hospital of Friendship Khmer-Soviet, Phnom Penh, Cambodia. Soo Ah Kim3Department of Obstetrics and Gynaecology, Faculty of Medicine, Chosun University, Gwangju, Korea. Gyeong-Eun Heo1Department of Obstetrics and Gynaecology, Soonchunhyang University College of Medicine, Bucheon, Korea. Abstract Vulva infections may present a differential complex to gynecologist, ranging from superficial skin infections to life-threatening necrotizing fasciitis. Recognition and timely treatment remain universal for skin and soft tissue infections, as subcutaneous vulva anatomy can facilitate rapid spread to other tissues with significant morbidity and mortality. Using a multidisciplinary approach of the equipment for the care of vulvar cellulite and abscess can guide the treatment of antibiotic therapies to a more aggressive surgical debridation. In this report, a case of vulvar abscess caused by meticillin-resistant staphylococococcus aureus (MRSA) is described in a postmenopausal woman with underlying diseases of bronchymiasis and atelectasis. IntroductionVulvar cellulite and abscess often present diagnostic and therapeutic dilemmas for the gynaecologist. Generally a presumptive diagnosis based on presentation, physical examination and risk factors for serious diseases guides initial therapy. Although cultures can be beneficial to direct specific coverage of antibiotics, in general, laboratory and imaging tests are less useful than an exhaustive story. Therefore, although these diseases can first present them to a gynecologist, a multidisciplinary approach is advocated to collaborate when necessary between the division of infectious diseases, the general surgeon and dermatology to maximize the accurate diagnosis and treatment of patients with vulvar and abscess cellulite. Case ReportA 56-year-old The Chinese woman, in the postmenopausal state of 6 years, visited the outpatient gynaecology department with the main complaint about a painful lump on the right side of the main laboratory. When examining, there was high fever with a body temperature of 38.9 °C, 120/minute pulse and 120/80 mmHg blood pressure. The pelvic examination revealed a steady, tender, swollen and inflated increase of labium major on the right side (). His laboratory work revealed a low hemoglobin of 10.5 g/dL, a high number of white blood cells of 17,140 with higher sedimentation rate of erythrocytes (ESR) 70. His hepatitis B serum, human immunodeficiency virus (HIV) and rapid plasma reanimation laboratory tests (RPR) were negative and the postmenopausal state was confirmed by the hormone test (estradiol [2] The results of the vaginal hysop to detect sexually transmitted disease (Trichomonas vaginalis, Mycoplasma hominis, Mycoplasma genitalium, Chlamydia trachomatis, Neisseria gonorrhea and Urea plasma urealyticum) were negative but Klebsiella pneumoniae (K. pneumoniae) was discovered. The Vulvar culture was identified as the presence of a lot of Staphylococcus aureus. After two days of antibiotics (cefotetano + metronidazol), he presented cough and hemoptissis then was transferred to the respiratory department. CT scan of the chest and bronchoscopy were performed with the result of bronchymiactasis in the left field of the upper lung (LUL) and Atelectasis in the right field of the middle lung (RML). Five days later, she was moved back to the gynaecology department and consulted with the infectious disease department, then antibiotics were changed to ciprofloxacin and trimethoprim-sulfamethoxazol. After 11 days of antibiotics combined with conservative therapy, he recovered completely () of his symptoms and the vaginal hysop was negative. Debate Increases the incidence of postmenopausal distress in women, who admitted to the emergency department. Menopause genitourinary syndrome (SMG) is a new term that describes several symptoms and menopausal signs associated with physical changes in vulva, vagina and lower urinary tract. Vulvar abscess is a common gynecological problem that has the potential to cause serious illness. These abscesses usually originate as simple infections that develop in vulvar skin or subcutaneous tissues. The loose areolar tissue in the subcutaneous layers and the contigüity of the vulvar fascial planes with the previous ingle and abdominal wall facilitate the spread of infection and the formation of abscesses in the vulvar area. Vulvar abscesses, including abscesses from the Bartholin gland, are often mixed polymicrobial infections, which consist mainly of MRSA, entérico graf-negative aerobes, and anaerobes of the female lower genital tract. Vulvar skin is colonized with organisms found in the skin and vagina and rectum. Staphylococcus aureus, esquerichia coli (E. coli) and other vulgative infictive organisms are commonly isolated from vulvar abscesses. Anaerobic bacteria, such as Peptostreptococcus or beta-lactamase-producing anaerobes (Bacteroides fragilis) may also be present in this polymicrobial infection. MRSA is the most common pathogen among vulvar abscesses that require incision and drainage. The main vulvar abscess management can be differentiated on the basis of the appearance or absence of an associated cavity of abscess, risk factors for rapid progressive disease, such as necrotizing fasciitis and systemic signs of disease. The Society of Infectious Diseases of America published in 2014 guidelines for skin treatment and soft tissue infections that offer comprehensive evidence-based recommendations based on a moderate, moderate, severe and organized classification by the presence or absence of a purulent abscess. If an abscess is present with mild cellulite without risk factors, treatment with antibiotics and serial surveillance after incision and drainage is reasonable. Due to the high prevalence of MRSA, antibiotic coverage should include this organism. The previous research has documented a high susceptibility of MRSA to trimethoprim-sulfamethoxazole, which also provides coverage to other commonly isolated microbes of vulva, such as Proteus, E. coli, and the B Streptococcus group. The duration of therapy is guided by the resolution of symptoms. The patient presented with inflammatory skin disease in the vulva should be considered of Lichen sclerosus (LS) which refers to a benign, chronic, progressive dermatological condition characterized by marked inflammation, epithelial slimming and dermaleal distinctive changes. LS is the risk of vulva squamous cell carcinoma by 4% to 5%. The diagnosis of LS is based on the presence of characteristic manifestations, ideally with histological confirmation. The ezrin is widely present on the vaginal wall. This has implications for the strength and resilience of this tubular structure and may be the case in other internal genital tissues. Although the composition of omega-3 fatty acid changed in the diet, the vaginal epithelial morphology did not change. Estrogen had effect on the vaginal cell, but omega-3 fatty acid had no effect on the ezrin and merlin vagina. In this case, we isolate Staphylococcus aureus from vulvar majora abscess in a postmenopausal woman, carrier of K. pneumoniae in vaginal flora, with underlying diseases of bronchitis in LUL and atelectasis in RML. Pneumonia belongs to the normal flora of the human mouth and intestine. K. pneumonia infections are usually hospitalized and are mainly produced in patients with impaired shelter defenses. The patient received antibiotics combined with conservative therapy (without incision and drainage) and a multidisciplinary approach to the infection department. From our finding in this case and comparing to literature, two interesting points were observed that a carrier of K. pneumonia in vaginal flora and vulvar abscess caused by MRSA in a postmenopausal woman, which is a rare case. Recent literature confirms an increase in the prevalence of MRSA skin acquired by the community and soft tissue infections. Outpatient treatment is more common in women with medical comorbidity, major abscesses and signs of systemic disease and MRSA was the most common organism isolated in women with vulvar abscesses. Although the MRSA acquired by the community is a virulent organism, most of the isolated MRSA were sensitive to trimethoprim-sulfamethoxazole. Vulva can be an area that is particularly susceptible to MRSA skin and a soft tissue infection. The gynecologist who evaluates a patient with vulvar abscess should consider the MRSA as a cause. An antibiotic regime should be initiated with activity against MRSA, such as trimethoprim-sulfamethoxazol, in similar populations with vulvar abscesses. Recognition This work was supported by the Soonchunhyang University Research Fund. Conflict of Interest: No potential conflict of interest related to this article was reported. ReferencesFormats: Share , 8600 Rockville Pike, Bethesda MD, 20894 USA
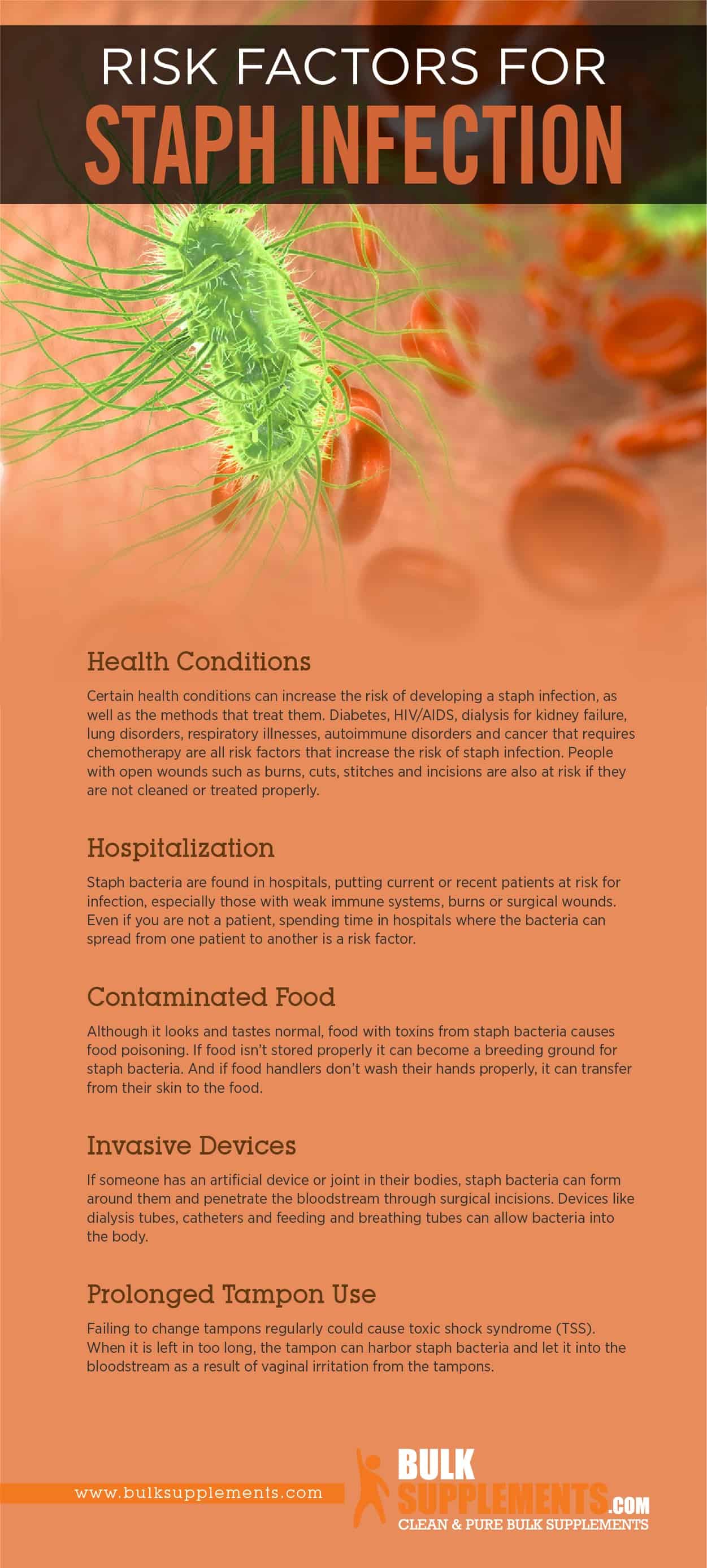
Top navigation MenuAccountMoreExplore Health.com Explore Health conditions A-Z News Diet and nutrition Fitness Beauty Mind " Body " Lifestyle Profile MenuAccountMoreFollow UsThe Truth About Staph When I heard that high schools were closing and teenagers were dying because of it, I felt lucky. Since mid-2006, Ive had resisted Staphylococcus Staphyloco aureus six times and somehow managed to avoid the worst: I have never been hospitalized and do not fear for my life. But please take my advice and do everything you can to prevent this dangerous infection. My first episode was in July 2006. I live in Boston and was going to visit a friend in Nantucket. I recovered in my seat on the plane and felt a boring pain, as if someone were pressing very hard on me. When I arrived I asked my friend to take a look. That sounds embarrassing, but I couldn't see the problem myself. He said it was just a very red one. On the third day the irritated area was more than three inches wide and burns sharply. I was nervous, so I left the island early and went to my doctor. He gave me an antibiotic called for a skin infection, but the grain became bigger, hotter, stronger and reder. Feeling was almost impossible. And soon it wasn't just my ass that lit up. I've developed a second place on my lips! Next page: [Pagina de página]What is it? I still didn't know he had MRSA. The truth is, I barely knew anything about the MRSA. But I wasn't going to get better, so while I was at my weekend home in Connecticut, I decided to go to the emergency room. The doctors gave me a , then cut and cleaned the place in my buttock. The abscess below was large enough that they had to pack with absorbing material to pack pus. When they finally knew it was MRSA. Doctors changed my antibiotic to Augmentin, because the first would not work against the resistant failure. But they didn't want to touch the place on my lips. I'd have to go to one for that. When I returned to Boston, I returned to my doctor's office to change the packaging, but the doctor wouldn't do it because they didn't have the necessary surgical tools. I had to go to the emergency room. I went to the emergency room in the same hospital complex; they agreed to change the packaging, but they didn't want to touch the place on my lips. They said they needed a gin again. Argh! Five doctors' visits to this infection, and the thing was getting worse. I was losing. I went into the medical building next door and found an OB-GYNs office. They agreed to take a look. The doctor painted the swollen area, pulled a little pus, and sent it to be cultivated. It was MRSA. Again. Both points were healed, and for three weeks it was fine. But then two months later, in September, it happened again: hot and red spots on my perineum and lips. I was really frustrated. I couldn't believe he'd come back. Before long I returned to the ER for another drainage and culture. More MRSA. More antibiotics, this time something called Bactrim. Next page: [page page page] Is it my fault? Eventually, I saw a , who did all kinds of tests (including diabetes and HIV) to find out if I had a condition that would make me vulnerable. It all went negative. I was surprised. I used to be a professional dancer, and I've always been very healthy. The tests, however, made me feel even more nervous and insecure about myself. The specialist couldn't explain why the shoots were still coming back, but the fact that they showed up where they sweated was a clue. I work at the gym three times a week and I also run. I came straight from the gym and would start working in the garden, changing the clothes first but waiting until I came back to shower. Bad idea. The specialist told me to take a shower and change my clothes immediately so that the bacteria would not have the opportunity to reproduce and wash me every day. She also made me try "decolonization"—a real nuisance. For five days, I was given an antibacterial soap called Hibiclens (also my husband), and for two weeks I put an ointment called Bactroban on my nose (because scam can live there) and on my perineum. I also washed all our sheets and towels every day, in hot water with bleach. Later, I saw a dermatologist who recommended me to change spandex to loose cotton only in case the tight suits were rubbing against my skin and leaving small abrasions. Next page: [page page page]What else can I do? I wish I could say that was enough to solve the problem. But last winter the infection returned—again!—this time under my arm and in my chest. My belly was next, in June, and again in September. Most of these points, like others, needed to be drained, packaged and treated with Bactrim. Did I do something wrong? My friends told me to change my doctor, but the doctors say the same thing: "They were seeing this a lot, and we don't know why their back." The truth is I feel like I was doing everything right. I'm obsessive now about following the advice of the specialists. I am humiliating in the hope of avoiding cracks on my skin that could be a breeding land. I wash my hands all the time. I use my wrists and my backs to open doors in public bathrooms. I can't imagine what else I could do with the MRSA. Except warn you. What are my real risks to MRSA?1 in 3.200 It is estimated that this year there is a chance to develop a serious MRSA infection, based on estimates of Centers for Disease Control and Prevention for the number of infections in 2007. Your chance of being audited by the IRS? One in 100. It is believed that up to 1 percent of Americans wear MRSA on their skin or on their noses, but most never develops an infection. In other words, their MRSA risks are extremely low, although no one can say for sure. In short, don't be scared, and don't put your head in the sand.* Jilly Jackson is not the real name of the authors. The book Maryn McKennas on MRSA, Superbug, will be published by Free Press in 2009. Participation options Log in Magazines & More informationConnectOther Meredith Sites View image

Genital Bullous Impetigo
Common Skin Infections: Common Skin Infections
Staphylococcus aureus Infections - Infections - Merck Manuals Consumer Version
Staph Skin Infections Pictures | How to treat boils, Home health remedies, Natural cures
Bullous impetigo in the genital area -intact and flaccid pustules,... | Download Scientific Diagram
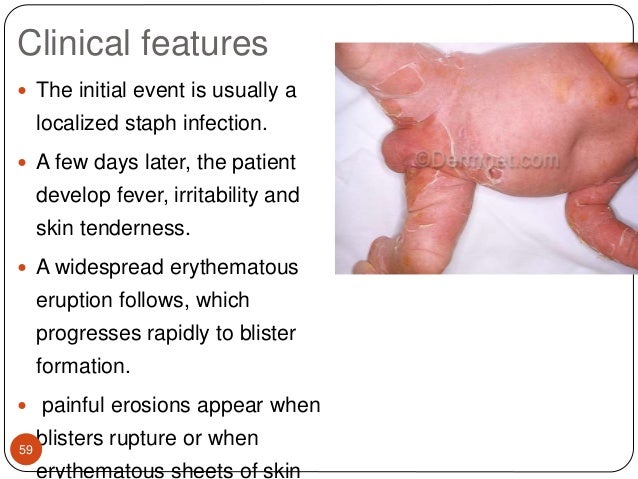
Staphylococcal Infections in Children: Part 1 | American Academy of Pediatrics
Infectious Disorders of the Lower Genital Tract - ScienceDirect
Skin and Soft Tissue Infections - American Family Physician
Itching and burning symptoms in the female urogenital tract | Publisso
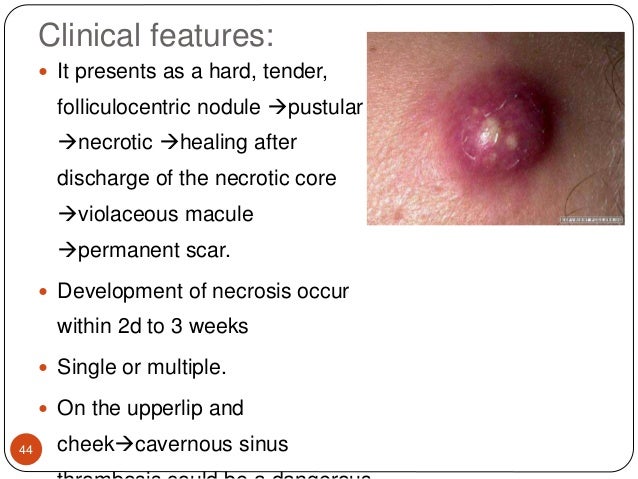
Diagnosis, Causes, and Treatments of Carbuncles
Folliculitis: Causes, symptoms, and treatment
Common Skin Infections: Common Skin Infections
Skin and Soft Tissue Infections - American Family Physician
Vulvar Aphthous Ulcer | Consultant360
Diagnosis, Causes, and Treatments of Carbuncles
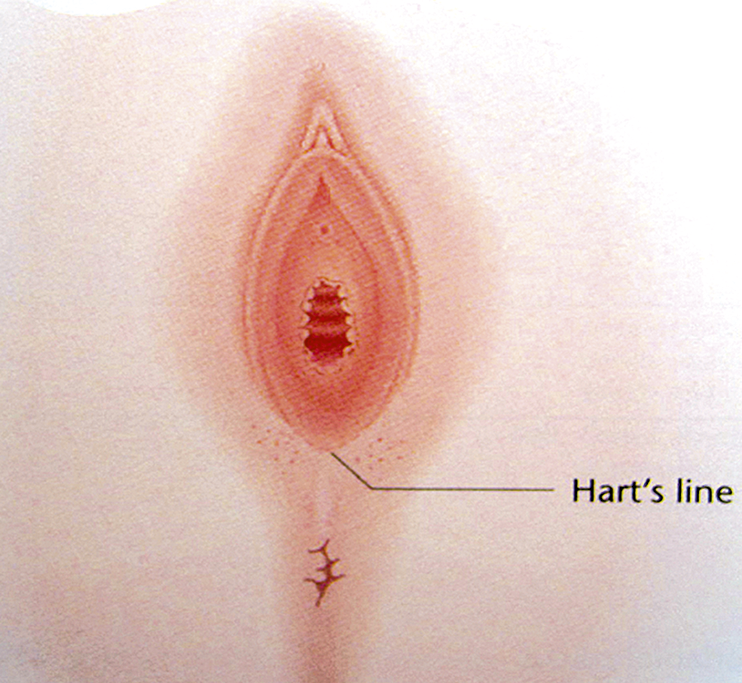
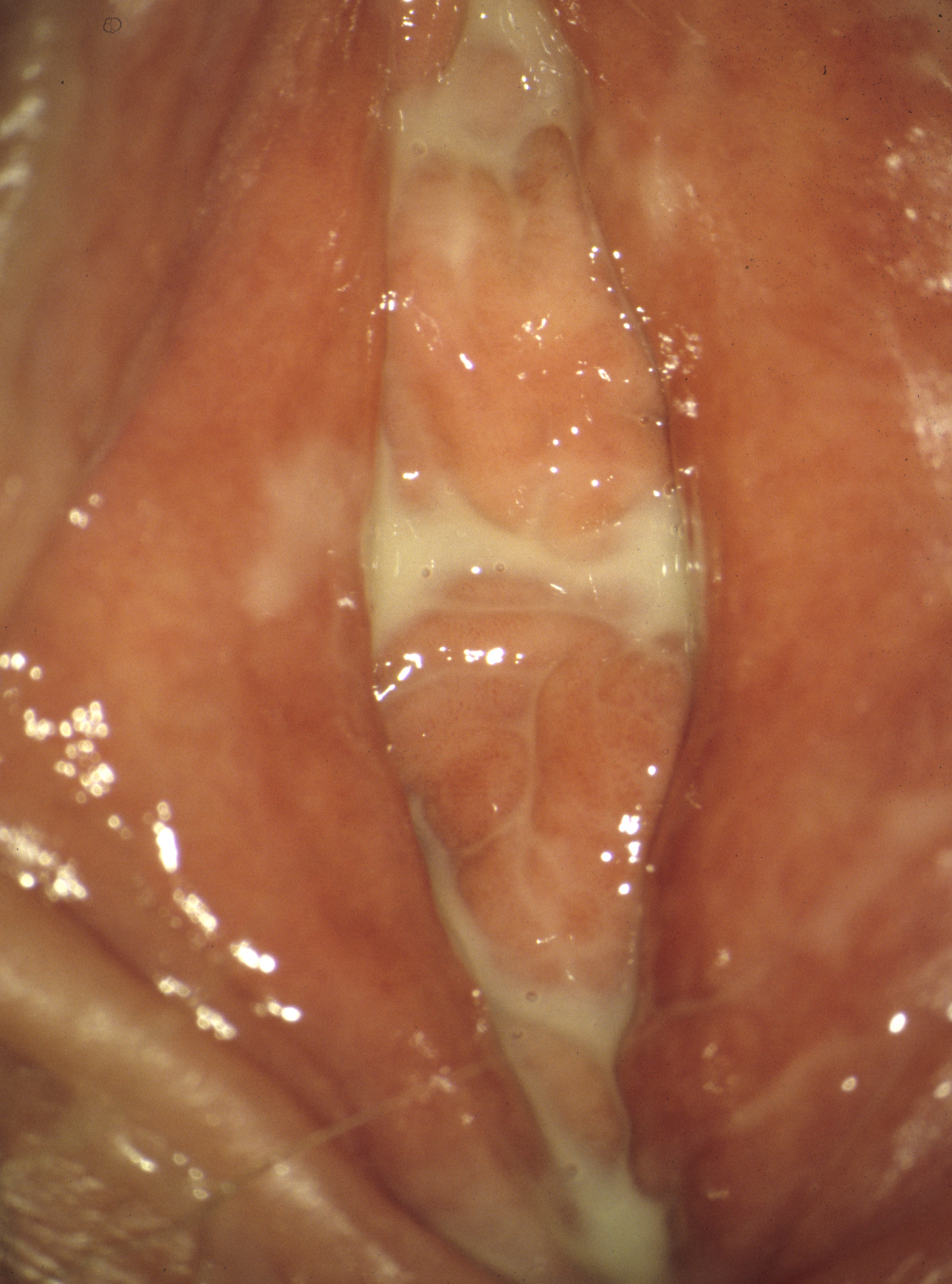
Colposcopy of the Vulva and Perineum | IntechOpen
Girlfriend let a staph infection get out of hand on her buttock : MedicalGore
Candida infection | DermNet NZ
Candidiasis - Wikipedia
How to tell genital herpes apart from other skin conditions.
The Most Common Infectious Diseases in the U.S.
Common Skin Infections: Common Skin Infections
Cellulitis - Skin Disorders - MSD Manual Consumer Version
Staph Infection and MRSA: Symptoms and Treatment - YouMeMindBody - Health & Wellness
The Most Common Infectious Diseases in the U.S.
Bartholin Gland Cysts - Gynecology and Obstetrics - Merck Manuals Professional Edition
Colposcopy of the Vulva and Perineum | IntechOpen
Staphylococcus (Staph) Infections: Symptoms, Risks & Treatment
Yeast Infection Sores & Blisters: Causes & Appearance | epicuriousmorsels.com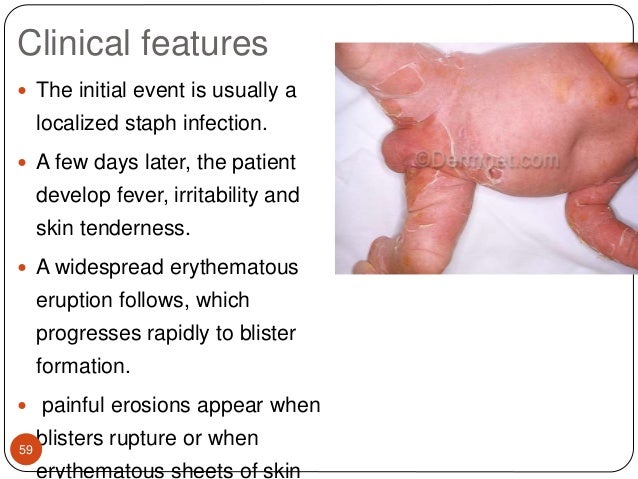
Staphylococcal & streptococcal skin infections
Staphylococcus aureus - Vulvar Disease - Global Healthcare
I think I have MRSA near my vagina. I'm scared. What do I do? | Center for Young Women's Health.jpg?width=252&height=168&scale=canvas)
Genital psoriasis, in images
Boil Treatment | Online Furuncle Treatment | i-GP Online Doctor
Vulvar Aphthous Ulcer | Consultant360
Staphylococcal infection - Wikipedia
4 Natural Ways Of Preventing Infection And Cleansing Vagina - So Healthy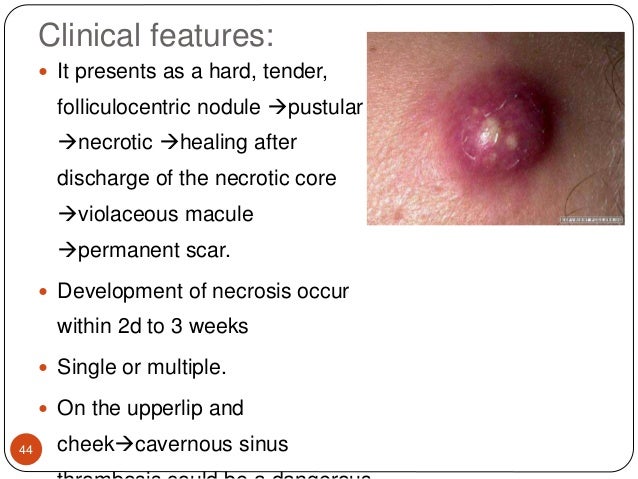
Staphylococcal & streptococcal skin infections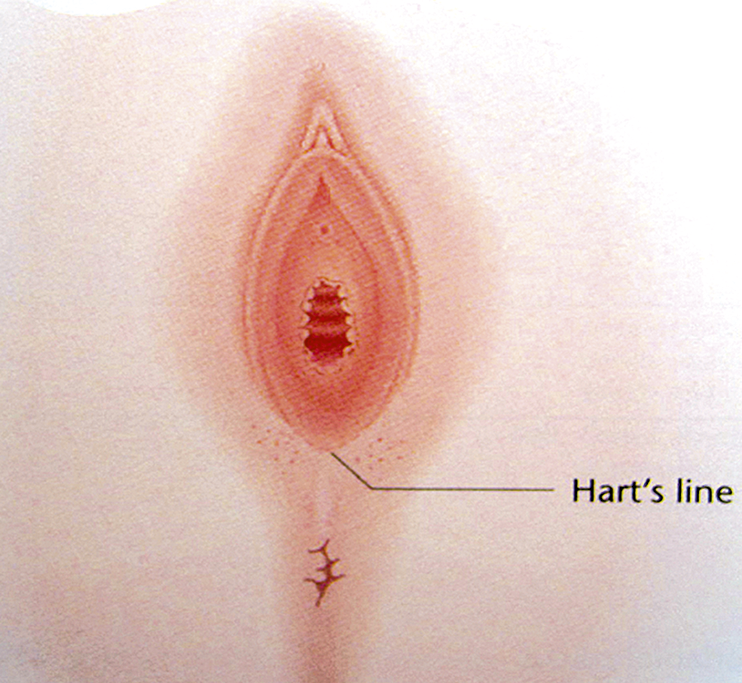
The vulva and vagina (Chapter 37) - Silverberg's Principles and Practice of Surgical Pathology and Cytopathology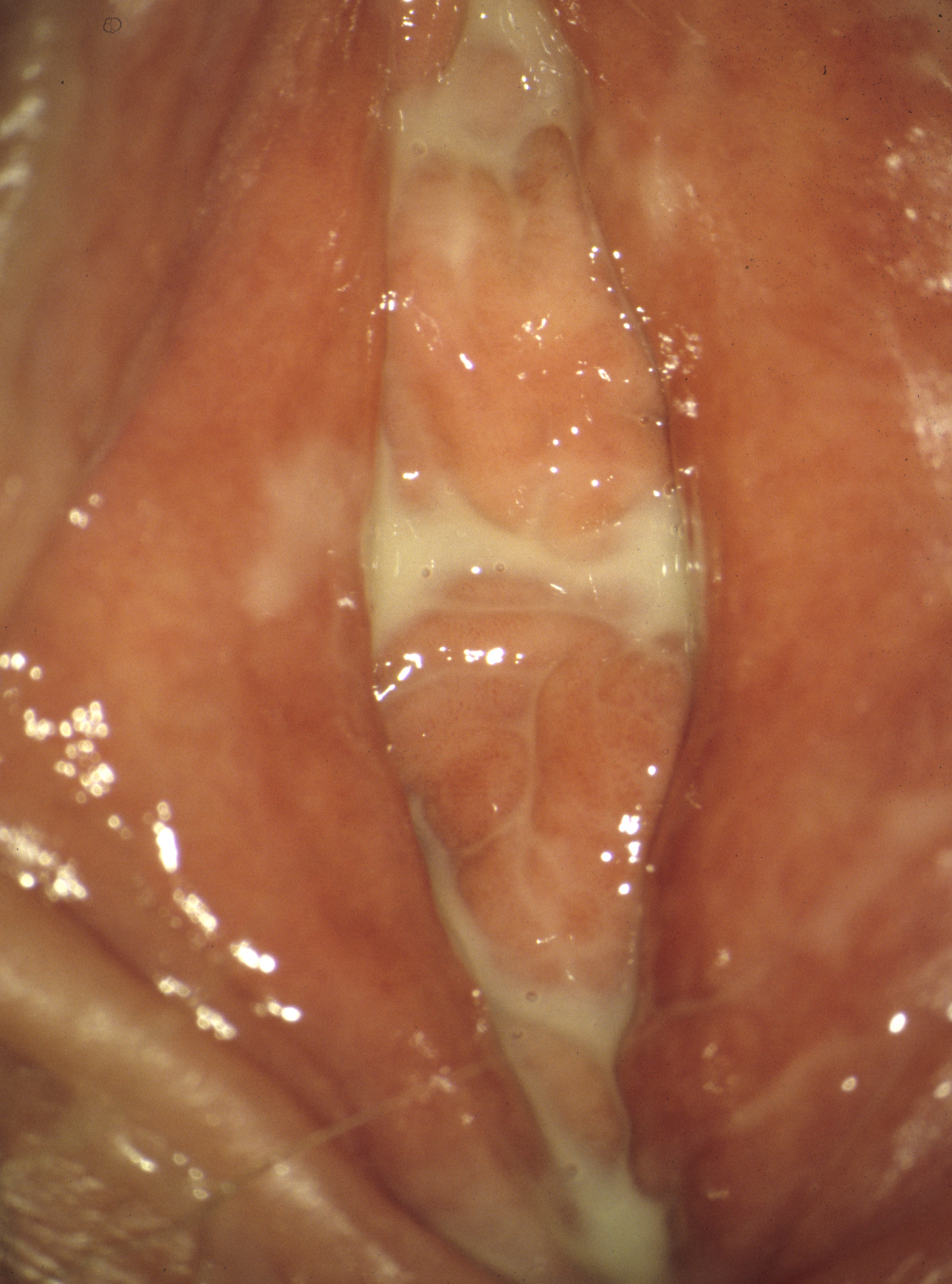
Itching and burning symptoms in the female urogenital tract | Publisso





























.jpg?width=252&height=168&scale=canvas)




Posting Komentar untuk "staph infection on labia"